Table of Contents
I. The Function of Blood Clots
II. How do Blood Thinners Work?
III. Conditions That May Require Blood Thinners
The Function of Blood Clots
The majority of us do not think much about the blood circulating within our bodies until we get a cut or scrape. Those little scrapes stop bleeding quickly due to coagulation factors in the body. Some people may experience problems with the clotting process, and dangerous blood clots may form. In most cases, your body will dissolve a blood clot after an injury, but in other cases, blood clots may break off in the blood vessels and travel to the heart, lungs, brain, or legs to cause serious medical events.
If you are at risk for blood clots, you may be prescribed blood-thinning medications like Xarelto (rivaroxaban), Elmiron (pentosan polysulfate sodium), Coumadin (warfarin), and Eliquis (apixaban). Read on to learn more about common blood thinners today. [1]
How do Blood Thinners Work?
Blood thinners are a super common prescription medication. Two to three million people a year take daily blood thinner drugs. These drugs help protect people against heart attacks and strokes when taken properly. Contrary to the name, blood thinners do not make your blood thinner, but they help break up clots and slow the growth of existing ones. There are two types of blood thinners available.
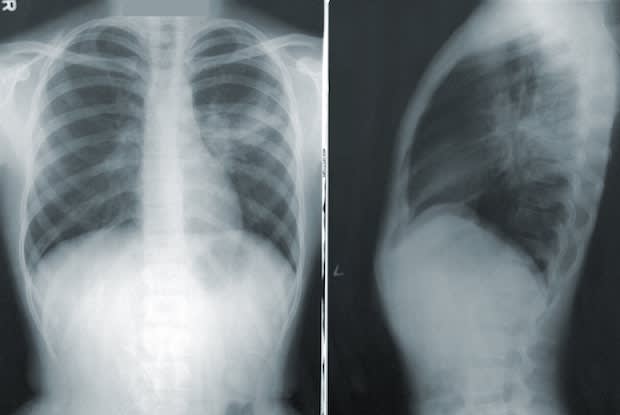
Anticoagulants work by inhibiting the creation of fibrin, which is a substance in the blood’s plasma. These drugs keep your blood from clotting or turning into a solid clump of cells that stick together. The majority of these drugs come in pill form. Anticoagulants work by interrupting the process involved in the formation of blood clots. Warfarin is the most common type of anticoagulant. Other common types of anticoagulants include: Platelets are tiny cell fragments that are essential for normal blood clotting. When a cut or injury occurs on the body, platelets rush to the wound site and become sticky, bind together, and form a clot to stop bleeding. This stickiness is beneficial for most cuts but can lead to clogged arteries. Antiplatelets make the blood less sticky and prevent arteries from becoming clogged. In some cases, antiplatelets and anticoagulants are taken together. Common antiplatelet drugs can include: Deep Vein Thrombosis (DVTs): DVTs are blood clots that occur in the vein and most commonly occur in the legs. This condition can be very dangerous, and you should seek medical help if you believe you are experiencing a DVT. You are at risk for DVT if you are confined to a bed, travel long distances in a car or plane, are pregnant, or recently had surgery that prevents movement. In some cases, DVT can occur for no reason. Possible symptoms of DVT include: History of Heart Attack: A heart attack occurs when a blood clot obstructs a coronary artery. These arteries supply blood to the heart, and if blood flow stops, heart muscles may die. Commonly, a clot can occur when there is plaque buildup in the artery. This buildup may break off or rupture the inner wall of the coronary artery. High cholesterol levels significantly increase your risk of a heart attack and plaque buildup. Symptoms of a heart attack include: Ischemic Stroke: Similar to a heart attack, an ischemic stroke occurs when blood vessels become narrowed or blocked. This reduces the blood flow to the brain and can cause serious side effects like brain damage, paralysis, or death. This blockage may also be caused by plaque buildup or blood clots that travel to the brain. Symptoms can include: Pulmonary Embolism (PE): A pulmonary embolism occurs when there is a blockage in the lungs' major arteries. Blood clots are the most common cause of PE. Clots can travel from the legs or other parts of the body. These medical events can be life-threatening, but prompt treatment can prevent serious consequences. Symptoms of PE include: It is essential to monitor your treatment when taking a blood thinner. Some medications like warfarin may require frequent blood testing, while others require less maintenance. Blood thinners always come with excessive bleeding risks, so you should stay on top of your maintenance appointments. Your doctor will decide the right type of blood thinner depending on your condition and risk factors. Blood clots are the most preventable type of blood condition, so medications like Xarelto (rivaroxaban), Elmiron (pentosan polysulfate sodium), Coumadin (warfarin), and Eliquis (apixaban) can significantly improve your quality of life and prevent serious medical events. [8] The content in this article is intended for informational purposes only. This website does not provide medical advice. In all circumstances, you should always seek the advice of your physician and/or other qualified health professionals(s) for drug, medical condition, or treatment advice. The content provided on this website is not a substitute for professional medical advice, diagnosis, or treatment.
a. Anticoagulants
b. Antiplatelets
Conditions That May Require Blood Thinners

Blood Thinner Maintenance
